ECMO stands for Extracorporeal Membrane Oxygenation. It is a kind of life support where the heart, lungs, or both are supported by pumping blood that is high in oxygen using a machine. A patient whose own heart or lungs are unable to pump enough blood or oxygen into the blood can have an artificial heart and lung provided by the ECMO system. ECMO is used after other methods of supporting the heart and lungs did not work. A patient’s heart and lungs may “rest” while ECMO takes over, so you might see an improvement after they are on it. The goal of ECMO is to let the heart and lungs recover while the patient is supported by the ECMO machine.
Dr. Virendra Singh, a renowned expert in critical care offers an insightful guide on ECMO (Extracorporeal Membrane Oxygenation) for both healthcare professionals and patients. His guide provides a thorough explanation of the complexities of ECMO, a life-saving technique that helps patients whose lungs are malfunctioning to sustain breathing for extended periods of time. In addition, he highlights the need for cautious monitoring throughout ECMO therapy, possible hazards, and patient selection criteria.
COPD Specialist, Asthma Specialist, ILD Lung Specialist, Sleep Apnea Specialist
Access Needed For ECMO
To attach the ECMO circuit to a patient, one to three cannulas (tubes) are required. A tiny incision will be made by the surgeon, typically on the right side of the neck. Typically, a tube is inserted into the jugular vein through the tiny incision on the right side of the neck. Occasionally, a second tube is inserted into the carotid artery, another neck vessel, via the same little incision. These tubes are then connected to the ECMO machine. The blood vessels that were used for this treatment may be permanently shut off and unavailable for use in the future. In the neck, there are three additional arteries and three additional veins that typically carry blood and oxygen to the brain. Sometimes other sites may be used. For certain people, the tubes are inserted straight into the right atrium of the heart and the aorta, which is the main artery that leaves the heart. The ECMO machine is then attached to these tubes. Following the ECMO course, these blood arteries are restored rather than cut off.
Types of ECMO
ECMO can offer a variety of forms of assistance. Veno-venous ECMO (VV ECMO) is a type of ECMO used to support a patient’s lungs alone. This kind of ECMO is designed to give the lungs some rest rather than assist the heart. Blood is removed from the right side of the heart (right atrium), oxygen is supplied, and the blood is then returned to the right atrium where the heart pumps the blood to the body and lungs if a child is placed on ECMO just to maintain the lungs. Other patients are put on veno-arterial ECMO (VA ECMO), which supports their heart and lungs. If a child is placed on ECMO to support the heart, the blood is taken out of a vein and returned to an artery.
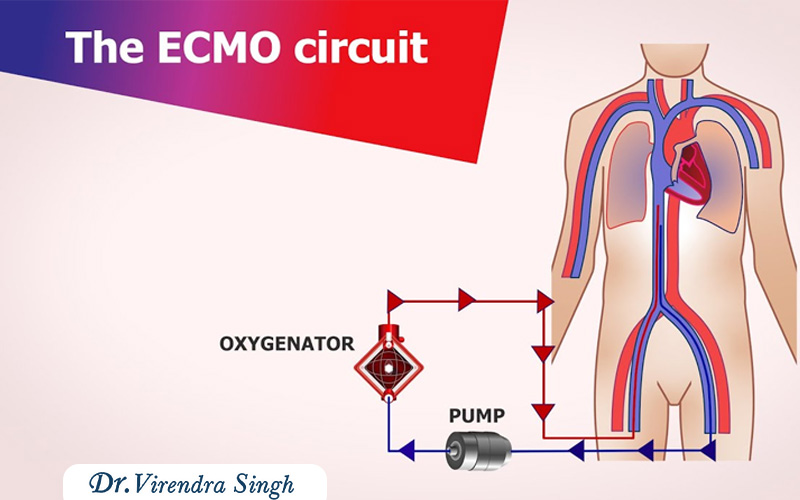
How ECMO Works
Blood is drained from the jugular vein tube to the ECMO machine via the tube. The blood can then be pumped by the ECMO system. An oxygenator, a type of artificial lung, is used to pump blood. By doing this, the blood’s carbon dioxide content (waste gas) is reduced and oxygen is added. As the blood passes through the oxygenator’s heat exchanger, it warms to body temperature. Blood that is rich with oxygen is then returned through the tube in either the carotid artery or jugular vein. The child’s blood will be dark crimson due to low oxygen levels. Usually, the blood returning will be more vibrant red (with oxygen).
1. Medicines :-
- When a patient is on ECMO, heparin (HEH par in) or a comparable medication is administered to prevent blood clotting in the tubes. Antibiotics may also be given to treat infection.
- Pain medicine or a sedative may be given. We employ these medications in an effort to maintain patients’ maximum level of comfort while they are on ECMO. Older kids and adults tell us that having ECMO is virtually pain-free. To assist us keep the tubes as straight as possible and enable the equipment to function properly, some patients may also be given medication to prevent them from shifting.
2. Blood Administration During ECMO :-
During ECMO, we will be giving blood products through the ECMO circuit. To replace the blood drawn for laboratory testing, new blood is administered. To assist stop bleeding, platelets—the component of blood that aids in clotting—are frequently administered. Please see Helping Hand HH-11-122, blood transfusion.
3. Nutrition :-
Intravenous (IV) fluids are typically given to ECMO patients as nourishment. During ECMO, feedings via a tube (inserted via the mouth or nose and into the stomach) may begin. While using an ECMO, some patients will be permitted to consume normal meals. Regular feedings will begin as soon as feasible following ECMO. As the patient gains strength, he or she may begin nursing, taking a bottle, or adhering to a doctor’s orders for a regular diet.
4. Tests Done During ECMO Therapy :-
- When the child is on ECMO, an ultrasound scan of the head may be performed every three days for the first three days, and then more frequently as needed to monitor for brain hemorrhage.
- Every day, chest X-rays will be performed to monitor any changes in the lung and the positioning of the ECMO tubes. The lungs may improve faster than the chest X-rays show. This is due to the fact that X-rays don’t always detect improvement right away.
- Laboratories that use blood gas Verify the blood’s oxygen content. A tiny blood sample is taken from the arterial line. The levels of carbon dioxide and oxygen are then determined. This enables us to modify the ventilator (breathing machine) and ECMO machine as necessary.
- Every hour, a tiny volume of blood will be drawn from the ECMO circuit to measure the blood clotting time. To avoid blood clots, the dosage of the anticoagulant or heparin may then be changed. In rare cases, Heparin may cause a patient to bleed excessively, in which case they will need to be removed from ECMO.
5. Weaning from ECMO :-
Weaning is the process of gradually returning to normal.
- Blood flow via the ECMO machine will decrease and ventilator assistance will rise as the heart and lungs get healthier and can pump more oxygen on their own.
- A patient’s ECMO tubes will be removed by the surgeon after they are able to maintain themselves with minimal assistance from the ventilator.
- The incisions will be closed with stitches and covered with a bandage.
- The tiny scar will gradually get better but won’t go entirely.
- Then we will begin slowly weaning the ventilator.
FAQs
What is ECMO?
Extracorporeal Membrane Oxygenation, or ECMO, is a life-support method used to give patients whose hearts and lungs are unable to adequately oxygenate their blood, prolonged cardiac and respiratory support. The procedure entails forcing the patient’s blood through a membrane-like artificial lung to exchange carbon dioxide for oxygen.
When is ECMO used?
Cardiogenic shock, cardiac arrest, severe respiratory failure (such as ARDS), and some surgical procedures are among the crucial circumstances when ECMO is commonly utilized. When the patient’s condition is life-threatening and traditional medicines have failed, it is frequently taken into consideration.
How does ECMO work?
A cannula, or thin tube, is used to withdraw blood from the patient’s body during ECMO. The blood is then passed through a membrane oxygenator, which adds oxygen and eliminates carbon dioxide, before being put back into the patient’s body. This process can assist in maintaining oxygen levels and reduce the workload on the heart and lungs.
What are the risks associated with ECMO?
Bleeding, infection, blood clots, and issues with the cannulation sites are among the risks associated with ECMO. Close monitoring and management are essential to minimize these risks.
Can ECMO be used for children and infants?
Yes, ECMO can be used in pediatric patients, including infants. The method and apparatus can be modified according to the patient’s dimensions and state.
